What Is Intestinal Dysbiosis?
Intestinal dysbiosis refers to the loss of beneficial bacterial mass or intestinal microbiota. It is a very common problem in the population that is related to the appearance of autoimmune diseases, inflammation, allergies, obesity, among other chronic diseases. Why is it produced?
First of all, it is necessary to take into account that the intestinal flora has been considered an organ in recent years. This is because it has diverse functions that influence the state of health and the metabolism of nutrients.
What is the microbiota? the state of symbiosis and intestinal dysbiosis
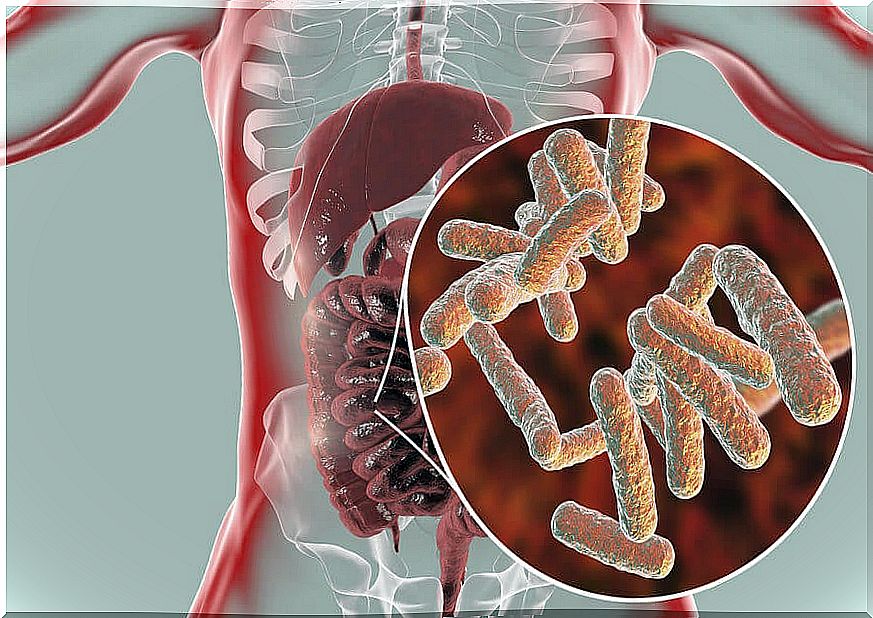
To begin, you need to talk about what it is. The microbiota is a community of different microorganisms distributed throughout the human body (skin, mouth, eyes, genital areas and, abundantly, in the intestine).
These populations form a mutually beneficial relationship with the host, known as symbiosis. This is demonstrated by a study published in the World Journal of Gastrotenterology . When there is an imbalance and a relationship is detrimental, we speak of intestinal dysbiosis. Many people refer to the gut microbiota as a “metabolic organ” as it contributes to:
- In the first instance, preserve the integrity of the mucosa.
- Is the first barrier to pathogens such as E . Coli.
- In turn, it regulates the functions of the cells of the immune system.
- It favors the synthesis of vitamins such as K, D and complex B.
Characteristics of the gut microbiota
The composition of the microbiota is quite complex and can undergo changes (acute or chronic) due to exogenous factors (such as lifestyle, habits, interaction with pathogens and / or chemicals, environmental agents) and endogenous factors (genetics).
Interestingly, it is known that there are more microorganisms in the human body than cells. Specifically, more than 1000 bacterial species live in the body (100 billion bacteria), although, predominantly, those of the phylum Firmicutes and Bacteroidetes are found.
The human microbiota
The growth of the microbial population that colonizes the intestine occurs from birth; it is strengthened with vaginal delivery and exclusive breastfeeding up to 6 months. With food and interaction with the environment, changes begin to emerge in the composition of the microbiota, which will define the health of the individual.
According to a study published in the Revista Española Endocrinología Pediátrica by Tinahones F et al, the predominant microorganisms in the human gastrointestinal tract are:
- Stomach: Helicobacter pylori (Proteobacteria), Lactobacillus (Firmicutes), Streptococcus (Firmicutes)
- Duodenum : Bacteroides (Bacteroidetes), Lactobacillus (Firmicutes), Streptococcus (Firmicutes), Staphylococcus (Firmicutes).
- Jejunum: Bacteroides (Bacteroidetes), Lactobacillus (Firmicutes), Streptococcus (Firmicutes), Bacillus (Firmicutes).
- Ileum: Bacteroides (Bacteroidetes), Clostridium (Firmicutes), Enterobacteriaceae (Proteobacteria), Enterococcus (Firmicutes), Lactobacillus (Firmicutes), Veillonella (Firmicutes).
- And finally, colon: Bacteroides (Bacteroidetes), Bacillus (Firmicutes), Bifidobacterium (Actinobacteria), Clostridium (Firmicutes), Enterococcus (Firmicutes), Eubacterium (Firmicutes), Fusobacterium (Fusobacteria), Peptostreptococcus (Firmicutesum Firmicutes) , Streptococcus (Firmicutes).
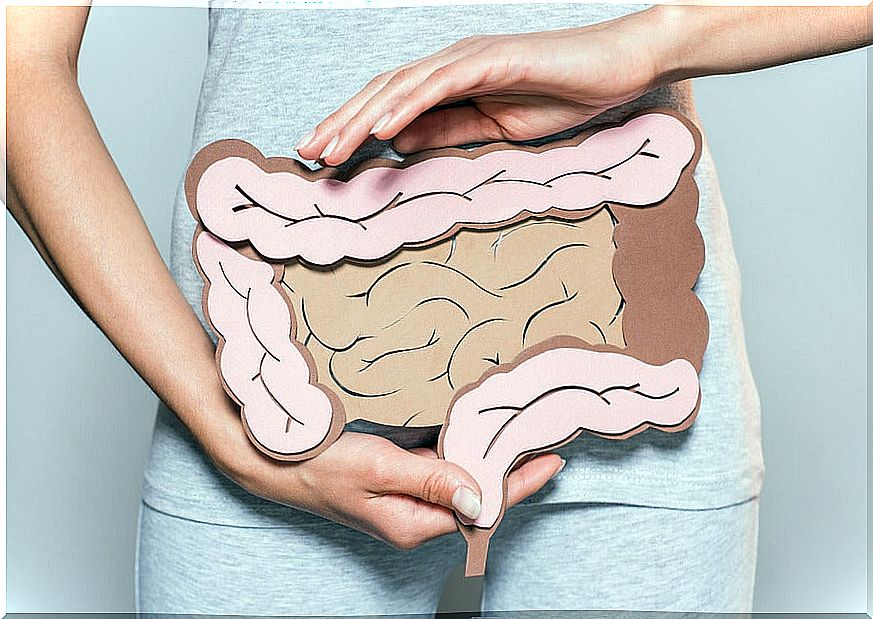
What is intestinal dysbiosis?
It is known, thanks to numerous studies, that the microbiota (specifically the intestinal microbiota) plays an important role in the functions of the organism and, when populations are altered, it promotes the development of diseases.
We speak of intestinal dysbiosis when there is an imbalance between the structure and composition of the microbial populations present in the intestine. When the microbiota is altered, it can contribute directly or indirectly to the development of numerous pathologies.
Gut-brain axis and gut microbiota
The gastrointestinal tract and the nervous system are intimately connected through the axis known as the “gut-brain “; a complex bidirectional system in which the enteric and central nervous systems interact with each other, developing through endocrine, immune and neurological circuits.
This has led to multiple theories about the multifactorial origin of neuropsychiatric diseases (such as autism spectrum disorders and depression), metabolic (such as diabetes and obesity) and tumor (such as colorectal cancer).
Characteristics of the gut-brain axis
Recent studies refer to a strong relationship between the gut-brain axis and the composition of the gut microbiota with the development of multiple diseases. Specifically:
- It is known that there are neuronal signals that influence motor, sensory and secretory functions within the gastrointestinal tract that, in turn, regulate inflammatory processes and the structure of the microbiota.
- Furthermore, intestinal signals can regulate functions within the nervous system.
Relationship between intestinal dysbiosis and obesity
According to a study published in Nutrients by Niccolai E et al, when the body is subjected to chronic stress, a load of cortisol is released that alters the permeability of the intestine and its protective barrier. Therefore, the composition of the microbiota is affected, generating intestinal dysbiosis. As a consequence, the intestinal microbiota produces alterations:
- Starting with the neurotransmitters that regulate appetite and satiety signals (such as serotonin).
- Increases the production of inflammatory cytosines.
- Produces alterations in the fat reserve
These changes trigger a favorable environment for the development of important metabolic alterations and an unbalanced eating behavior.

Importance of keeping the microbiota in balance
Finally, it is essential to emphasize the importance of maintaining an adequate composition of the microbial population in the intestine. In this sense, it is known that the characteristics of the diet and genetic factors decisively influence its structure.
Thus, a varied diet, with a high consumption of vegetables, fruits, grains and whole seeds, provides fiber as the main food for intestinal bacteria.
Taking care of the consumption of processed foods, high in sugars or sweeteners, as well as managing stress through the practice of meditation and exercise, are important measures to avoid intestinal dysbiosis.