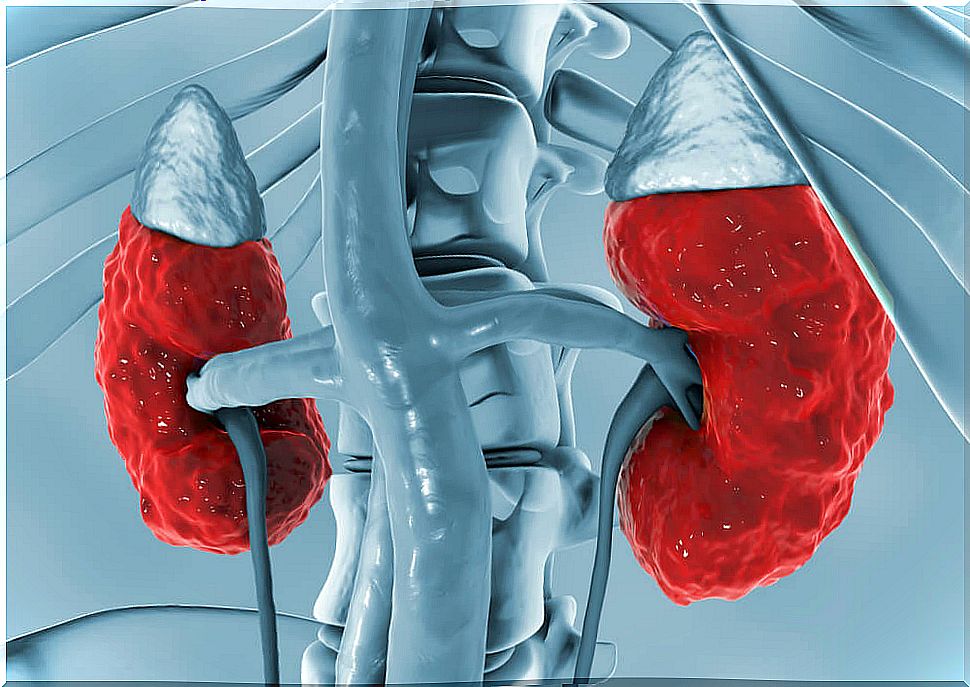
Causes Of Hyperchloremic Renal Acidosis
Hyperchloremic renal acidosis is caused by the loss of too much sodium bicarbonate from the body. Also, the kidneys do not remove enough acid from the body.
It is characterized by a decreased ability of the proximal tubules to reabsorb bicarbonate from the glomerular filtrate, resulting in hyperchloremic metabolic acidosis.
Its prevalence is unknown. However, drug-induced proximal renal tubular acidosis (pRTA) is relatively common. However, isolated hereditary hyprechloraemic renal acidosis is very rare.
Symptoms of hyperchloremic renal acidosis
The symptoms of hyperchloremic renal acidosis depend on the underlying disease or condition. This condition causes rapid breathing, lethargy, or confusion. Furthermore, it can lead to shock and even death.
Initially, it shows up with very basic urine due to the non-reabsorbed bicarbonate. There is also a delay in growth and a reduction in bone mineral density due to hyperchloremic renal acidosis.
In some cases, hypokalemia may occur and, occasionally, symptoms of periodic paralysis may develop. However, rickets and osteomalacia are due to vitamin D deficiency and lack of phosphate reabsorption.
Causes
Hyperchloremic renal acidosis can be caused by kidney diseases, such as distal renal acidosis and proximal renal tubular acidosis.
It can also appear in cases of poisoning with acetylsalicylic acid, ethylene glycol or methanol. In addition, it can appear if there is severe dehydration.
Hyperchloremic renal acidosis can be acquired or inherited recessively, in most cases, or dominant. Acquired renal acidosis is caused by a mutation in the SLC4A4 (4q13.3) gene.
However, dominant acidosis is caused by mutations in an as yet unidentified gene. The proximal mound reabsorbs about 80% of the filtered bicarbonate load, but a defect in it causes the loss of bicarbonate.
Also some drugs can be the cause of the development of acquired renal acidosis.
Diagnosis of hyperchloremic renal acidosis
Unlike patients with distal renal acidosis, those with proximal renal acidosis retain the ability to lower urine pH below 5.5
To diagnose the disease it is necessary to demonstrate the lack of bicarbonate reabsorption. The diagnosis is confirmed with a bicarbonate titration test.
In the titration test, an exaggerated increase in urinary bicarbonate excretion and urine pH will be observed as plasma bicarbonate rises above the renal threshold.
It is also necessary to exclude other inherited proximal tubulopathies, such as eye-brain-kidney syndrome, Dent’s disease, and GLUT2 deficiency glycogen storage disease.
An arterial blood gas and electrolyte analysis may be ordered as laboratory tests to confirm hyperchloremic renal acidosis.
In addition, a basic metabolic panel can be ordered, which consists of a group of blood tests that measure sodium and potassium levels, kidney function, and other chemicals. In turn, urine pH, blood and urine ketones and lactic acid levels are assessed.
This set of tests can also help determine whether the cause of acidosis is a respiratory problem or a metabolic problem.
Treatment
Treatment of hyperchloremic renal acidosis depends on the cause of the disease. Inherited proximal renal acidosis requires lifelong bicarbonate replacement therapy.
To carry out this treatment, a large amount of bicarbonate is needed to normalize the bicarbonate in serum.
In some cases, diuretics of the thiazide family are used in doses of 25-50 mg daily. For example, hydrochlorothiazide. This is done in order to improve bicarbonate reabsorption, thereby reducing the amount of bicarbonate required.
It is also necessary to monitor the plasma potassium level, which is why in some cases it is necessary to administer a mixture of sodium and potassium bicarbonate salts.
Drug-induced hyperchloremic proximal renal acidosis is usually reversible upon cessation of drug administration. With proper treatment, the prognosis for this condition is good.