Spinal Angiodysgenesis
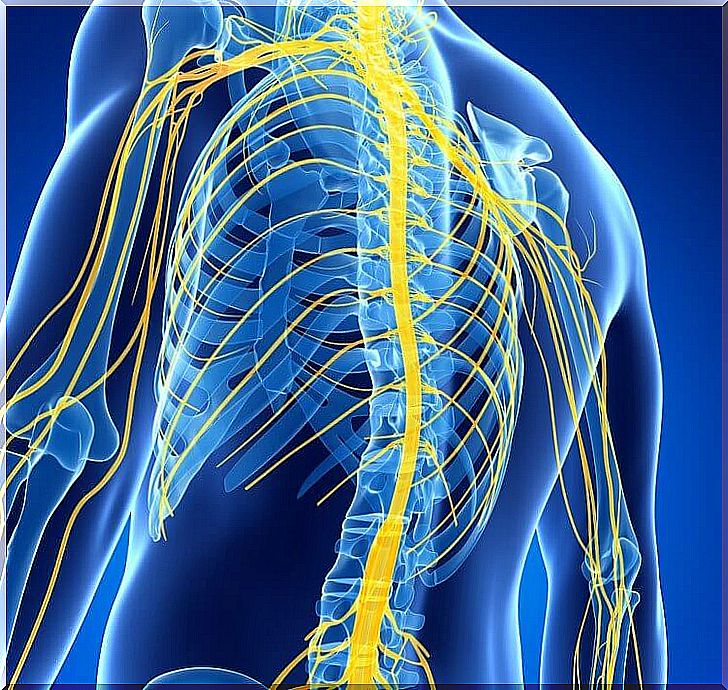
The spinal cord is a nerve tissue located in the vertebral canal. Its function is to carry nerve impulses and control immediate and vegetative movements, as well as the central, sympathetic and parasympathetic nervous systems.
Spinal angiodysgenesis is a term that encompasses the set of malformations of the blood vessels of the spinal cord.
This pathology arises from an abnormal embryonic development and is the result of a malfunction of the spinal irrigation.
Classification of spinal angiodysgenesis
According to radiological imaging tests, 3 types of spinal angiodysgenesis are distinguished, which we are going to see below.
Type I or predominantly adults
This is the most common type of all. An angiography of the spinal vessels revealed a single altered vessel.
The altered glass differs from the others because it is tortuous, that is, full of curvatures throughout its course. In addition, it usually occurs on the surface of the medulla.
Type II or glomus malformation
In this case, the involvement includes several small-caliber vessels.
These are always located in the same spinal segment in relation to the vertebrae. The altered vessels form a kind of vascular ball.
Type III or juvenile malformation
This type of dysgenesis is the closest to central nervous system angiodysgenesis. The surface involvement is more extensive, so it usually occupies several spinal segments.
These are several large-caliber vessels with rapid flow afferent to a central vessel. It is important to distinguish those malformations that are true from those that are only apparent:
- Dural arteriovenous fistulas. Those malformations in which the original nucleus of the lesion (known as nidus) is located in the dura mater covering the root.
- True vascular malformations. They have anatomical origin in some segment of the spinal cord. The nidus is found in the pia mater or in the medullary substance.
Characteristic signs and symptoms

Symptoms and signs are variable depending on the height of the vertebra in which the alteration occurs. In any case, the most frequent alterations are the following:
- Numbness.
- Muscular weakness.
- Tingling and other sensation disturbances.
- Root pain It is a type of pain radiating from the distribution of one or more nerve roots. For all this, it spreads in the anatomical regions that correspond to the area of skin innervated by the affected nerve root (the root is compressed and therefore pain appears).
- Segmental neurological deficit. The origin of this sign is due to compression of the spinal cord. They are not always permanent, they can appear and disappear alternately. However, the most common is that they are fixed and progressively evolve.
- Focal hemorrhage. It appears when the medullary parenchyma breaks. In an initial stage the parenchyma is compressed, but in the more advanced stages it is even replaced, resulting in rupture of vessels and the appearance of hemorrhage.
- Stiff neck and sudden headache. These are typical signs of arteriovenous malformations located in the first cervical vertebrae.
Diagnosis
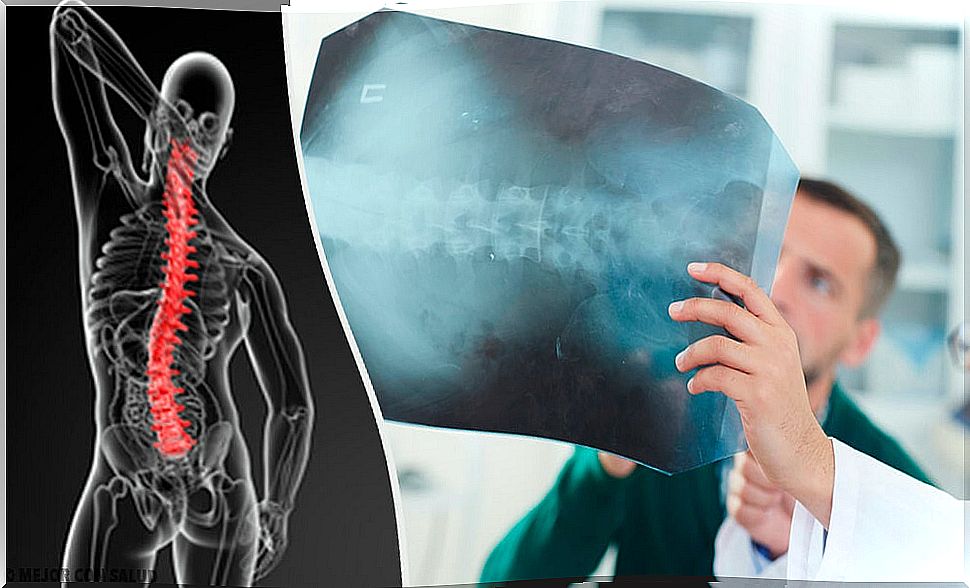
Diagnosis is made using imaging techniques.
Nowadays, radiography is not as relevant as it was a few years ago because alterations do not always appear (only 5% of arteriovenous malformations appear with radiological defects) and when they do, they are very unspecific manifestations (bone erosions and widening of the interpeduncular space).
Myelography is a widely used diagnostic test. This study consists of injecting radiofluorescent contrast into the patient’s body and observing in real time how it moves, following the path of the vessels and nerves of the spinal column.
The most striking feature, when there are arteriovenous malformations, is that the vascular structures appear thickened and tortuous, that is, their course has many curvatures.
Nonspecific findings may also appear, such as contrast depletion defect, spinal widening, arachnoiditis (inflammation of the arachnoid meninx), and subarachnoid block.
Treatment of spinal angiodysgenesis
Once the disease has been diagnosed, complementary tests are carried out in order to plan the most appropriate treatment for each patient.
The most common is spinal angiography, where the involvement of blood vessels in the injured area is studied to plan surgery (provided that normal spinal function is altered).
Sometimes it is interesting to consider angiographic embolization. This is a less invasive technique than the surgical approach.
The problem is that surgery is only effective in very small lesions in which the blood supply is blocked and there is no need for further interventions. At present, advances in the investigation of this disease continue to be made.